50 communes
saturation
operating territories
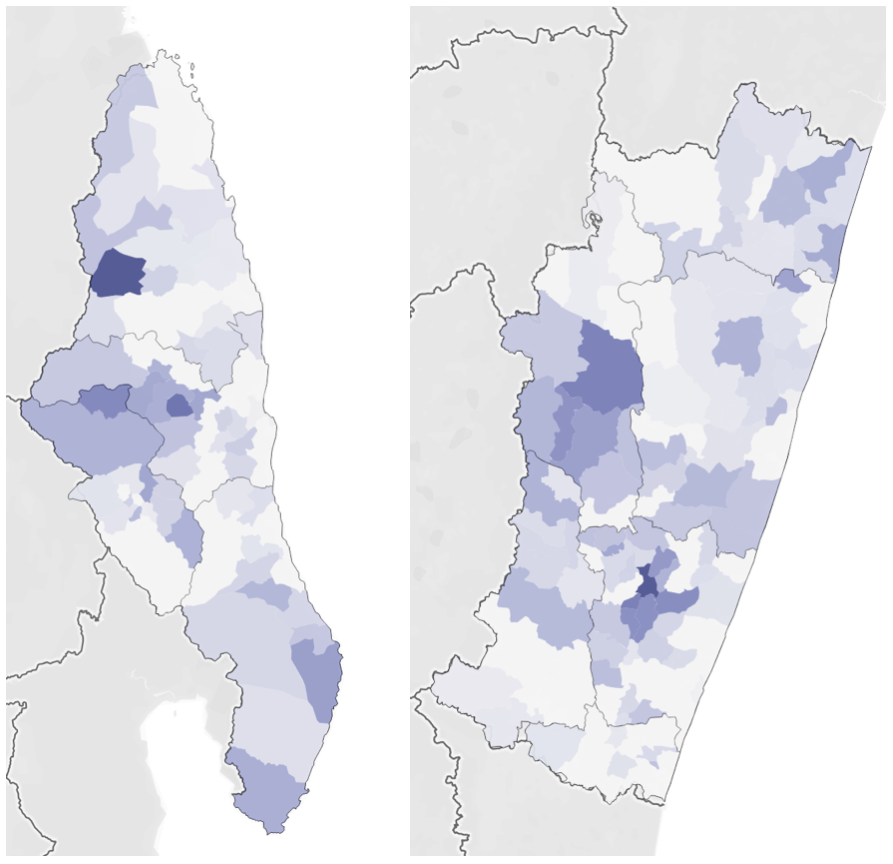
We are working directly with the Madagascar Ministry of Health to realize the vision for FREE in two regions (SAVA – on the left – and Vatovavy-Fitovanany, which we will refer to as V7V). These two regions are composed of 10 districts, and the 10 districts composed of 218 Communes. The first phase of our work is focused on 50 communes – 5 in each of the 10 districts.
To select the various Communes, we analyzed our saturation rate. We define saturation rate as the number of patients we have treated from the commune divided by the total number of estimated cases in the commune. The map to the left shows saturation rate by commune – the darker the commune, the higher the saturation rate. SAVA, left, has a maximum saturation of 37%, while V7V, right, has a maximum of 53%.
We want to prioritize saturation because we are closest to treating the entire backlog in the communes where saturation is the highest.
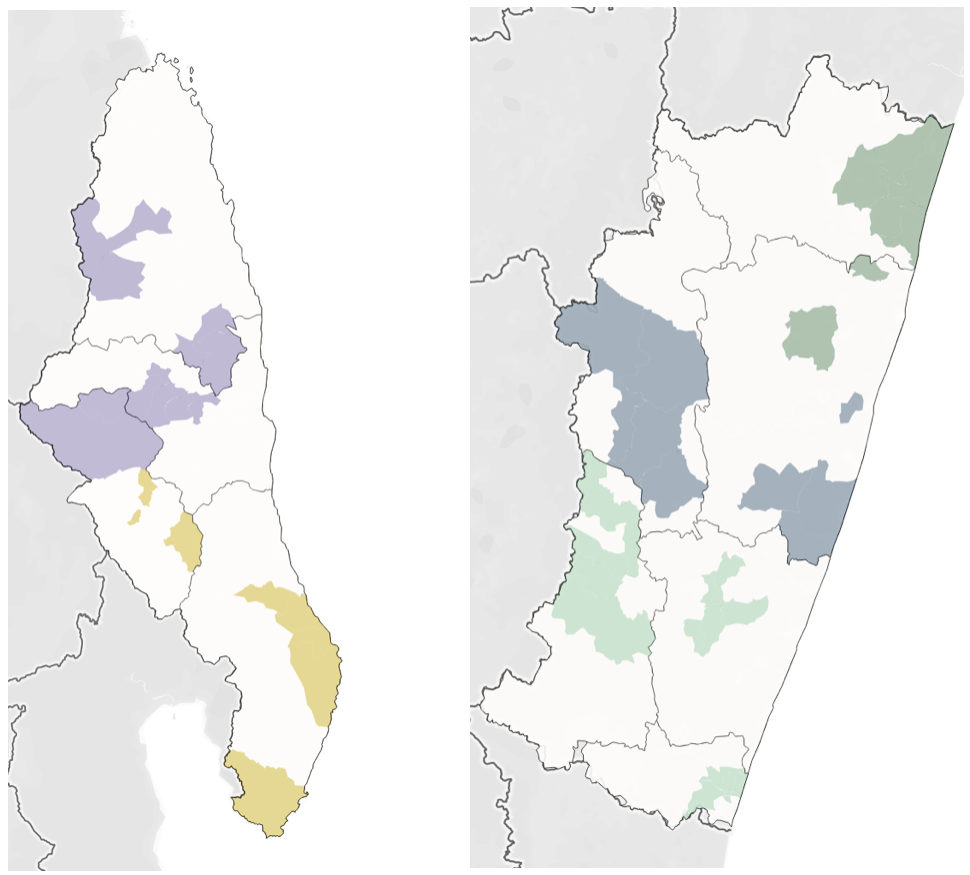
However, it is also important that we can function operationally in the selected communes. Roads, rivers, and mountains separate these administrative boundaries and so we must consider this geography.
Finally, it is important that we select a sample of communes that is diverse, so that what we learn in the project has maximum potential for replication, in Madagascar and beyond.
We first looked at implementation. In order to get program efficiencies, we clustered the 50 communes into 5 operating territories (SAVA North, SAVA South, V7V North, V7V Central, and V7V South), which you can see colored in the maps to the left.
We have selected all communes for diversity.
While we do not have a great deal of data on the different communes, we do have population estimates and land area. This allows us to understand size and population density. We broke the communes into quartiles by land area and population density, and tried to find balance across the quartiles.





